Public health experts in T.N. look back to the tumultuous year; say all safety precautions should continue
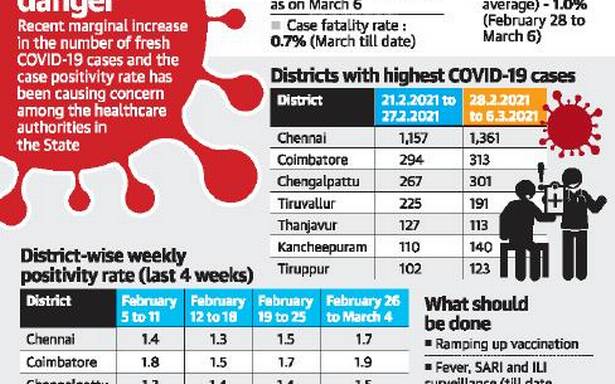
It has been a year since Tamil Nadu recorded its first case of COVID-19 on March 7, 2020. The State has come a long way in the control and management of the pandemic. But a rise in the number of fresh cases in a few districts has raised the level of alert.
As a sense of complacency has set in among the public, the emergence of clusters and continuing non-adherence to safety norms is posing a challenge for public health authorities. The journey has not been easy. In March 2020, the State’s positivity rate was 5.2%.
This rose to 10.5% in June, and went on to decline gradually from September, reaching 1.7% in December. After dropping below 1% in February 2021, for the first time since last March, the positivity rate is currently 1%.
Today, the State accounts for 8,54,554 cases, with 8,38,085 recoveries, 12,517 deaths and 3,952 active cases.
Between 50,000 and 55,000 tests are being done every day in the State.
“The last one year was a 360-degree challenge as it was not just a pandemic affecting the health sector but all sectors and individuals one way or the other. Initial phases of the lockdown helped in ramping up the health infrastructure. Clinical management improved tremendously, reducing the case fatality. Sticking to RT-PCR testing was unique to the State and helped in restricting the spread,” Health Secretary J. Radhakrishnan said.
Among an array of initiatives were the aggressive focussed testing, developing COVID-19 Care Centres to handle asymptomatic cases, setting up fever camps and screening centres for positive persons to decide who to send to hospitals, starting daily house-to-house surveys with pulse oximeters and thermal scanners, he said.
“Challenges of handling unlock with different levels of relaxation, the recent tendency to ignore masks and standard operating procedures [SOPs] considering the decline in the numbers after the peak in July and August, fatigue among people to adhere to public health guidance and not changing behaviour despite awareness are the challenges,” he said.
“We need to understand that while vaccination is a milestone, we need to continue to wear masks and avoid creating clusters by not being careless to the risks posed by newer variants,” the Health Secretary said.
T.S. Selvavinayagam, Director of Public Health and Preventive Medicine, listed various measures that helped in handling the pandemic during its peak — temporary appointments to support COVID-19 control activities, expanding bed capacity and oxygen beds, fever camps, triage centres, interdepartmental coordination and the conduct of serosurveys for epidemiological purposes.
“We moved from complete lockdown to unlocking because of the support from everyone, including the government and citizens. The same is needed for some more time. Otherwise, we will face further waves. COVID-19 appropriate behaviour should continue,” he said.
It has been a challenging year, Prabhdeep Kaur, Deputy Director of the Indian Council of Medical Research-National Institute of Epidemiology, said. “The State stepped up case detection, testing, hospital facilities and took several public health control measures, along with restrictions and lockdowns. In a nutshell, Tamil Nadu has done reasonably well when compared to many other settings,” she said.
According to T. Jacob John, retired professor of virology, Christian Medical College, Vellore, the State has not done too badly although there were some hiccups now and then.
“Due to the early high-handed response across the country, people were tired and became complacent when the time came for an actually needed high-handed response. There was a mismatch in the timing when we needed strict control measures and when we actually applied strict control measures,” he said.
With the rise in the number of fresh COVID-19 infections in specific regions, Dr. John calls for a need-based approach in vaccination that target these areas.
The main problem is that the risk perception was low, Dr. Kaur said. “We do not know whether a second wave will happen or not. The risk is high and the new variants have a tendency to spread faster. Wearing masks, avoiding crowding, trying to meet people in open spaces and getting vaccinated should be the priority.”
Dr. Kaur highlighted the need to detect clusters early. “If we need to prevent outbreaks, we will have to pick it early and do extensive contact tracing. Sustaining testing and tracing is key. We need to see if we are testing where we need to test — contacts, households and closed settings,” she said.
“While healthcare and frontline workers can be proud of what they could do despite severe scientific limitations in the initial period, there is still a long way to go before we can afford to relax,” Dr. Radhakrishnan added.
Source: Read Full Article