In the over one year since the pandemic began, the response has evolved. A look at what we have learnt so far, and the challenges that remain.
Family and friends often call to know which of the two Covid-19 vaccines available in India is better. My advice to take whichever is easily available is met with apprehensions about adverse effects of vaccines. This is symptomatic of the past year, a year full of half-truths, false claims and often outright lies that became more viral than the virus itself. While it has been a remarkable year for science and the value it brought to society, there is little understanding of the scientific method, which relies on data and evidence.
As India approaches one year of its lockdown, I review the year gone by and attempt some cautious crystal gazing into what lies ahead.
The early response
Our understanding of diseases and the germs that cause them has advanced by leaps and bounds starting in the mid-20th century. Yet, the initial human response to a disease outbreak has changed little. In his essay, What Pandemic Novels Teach Us, novelist and Nobel laureate Orhan Pamuk reminds us that “People have always responded to epidemics by spreading rumor and false information and portraying the disease as foreign, brought in with malicious intent.” Comparing Covid-19 to historical outbreaks of plague and cholera, he says, “There is an overabundance of similarities. Throughout human and literary history, what makes pandemics alike is not the mere commonality of germs and viruses but that our initial response has always been the same.”
In the past, rumours and false information were driven by not understanding a disease, but the new age tools of modern communications now aid that spread. As with old plagues, rumours and accusations based on nationalist and religious identities, fueled through social media, have impacted how Covid-19 unfolded in India and other parts of the world. Through the ages, the most common rumours were about who carried the disease and from where. The disease is always foreign, either brought with malicious intent or due to the incompetence of others to contain it in a foreign land. The Romans blamed Christians for their practices that angered the Roman gods and brought the Antonine plague of smallpox in 165-180 AD. In the early days of the HIV/AIDS epidemic in the 1980s, preachers and televangelists blamed it on the “perverted lifestyles” of homosexuals and concluded that “AIDS is God’s punishment”. Still others argued that the HIV/AIDS virus came about due to voodoo practices or that it came from outer space or was a bioweapon created in a CIA lab. In 2020, contrary to overwhelming scientific evidence that the Covid-19 virus was first transmitted from bats to humans and then from person to person, many still assert it was produced in a Chinese lab.
Denial has been another early response to disease outbreaks. Governments have distorted facts and manipulated data to first deny the disease and then cherry pick data to not reveal its full extent. This is always done in ‘public interest’. The denial by South Africa’s President Thabo Mbeki (1999-2008) that AIDS was caused by a virus, and the failure to provide available medicines to infected people caused hundreds of thousands of preventable deaths and new infections there. The continued denial of Covid-19 as a problem at the highest levels of the US government during the early part of the pandemic led to a grave situation in the world’s most technologically advanced nation. The country is now reeling with over 31 million cases and 568,000 deaths. With almost 13 million cases and over 330,000 deaths, Brazil also owes the devastation to early denial by its leadership. Sweden ignored guidance and tried controlling the pandemic by letting its population get infected to reach herd immunity. Despite an excellent healthcare system, Sweden registered 15 to 20 per cent mortality in April and May 2020, forcing it to abandon this strategy.
The nature of pandemics
Pandemics are caused by infectious agents but spread by humans. The control, therefore, depends as much on how humans behave as on medical intervention. When the populace trusts policy makers, it follows advice. Trust comes from transparency and clear and honest communication, all found wanting over the past year. For example, there is overwhelming evidence that masks prevent infection and save lives. In data from 200 countries, Covid-19 mortality was 100-fold lower in countries that implemented mask wearing within 15 days of first case detection compared to those that took 60 days or more to do so. Then why don’t people wear masks or wear them properly. The same goes for avoiding crowded places, known to spread infection.
People’s choices reflect the relative costs of illness and its avoidance to them. If this private cost of illness is low, or the private cost of avoiding illness is high, people have little incentive to follow preventive measures. It is hard to convince someone who has no food security to wear a mask. It is impossible for the poor to practice ‘social distancing’ while trying to earn a living or within their crowded dwellings. The essentially economic nature of individual decisions, and the role of behaviour and economics in epidemiology determines the societal impact of a pandemic. One of the biggest gaps in the global response to the pandemic is the understandable reliance on technological solutions, with insufficient attention to communications, human behaviour and social networks.
Though microbes infect royals and commoners alike, pandemics are unequal in their impact. The “Spanish Flu” of 1918-20claimed about 50 million lives of which 12 to 18 million are thought to be from India, which was under colonial rule. The mortality rate in Britain was 0.47 per cent, for Europeans living in India it was 0.83 per cent, but for Indians it was 2 per cent. Even among Indians, lower castes and upper castes showed 6.1 per cent and 1.9 per cent mortality, respectively. In South Africa under apartheid 32 per cent of the white population was infected with 0.8 per cent mortality; 46 per cent of blacks were infected with 3 per cent mortality.
Poverty and unequal access to healthcare creates such disparities. Covid-19 may not be very different in this respect. While the overall life expectancy in USA fell by one year in the first half of 2020, for the black population it declined by 2.7 years in the same period. The life expectancy gap between black and white Americans is now at six years, the widest it has been since 1998. Considering its very large informal workforce and poor healthcare infrastructure, India is unlikely to fare any better when reliable data becomes available.
The pandemic in India
When India went into a lockdown on March 25, 2020, there were 525 confirmed cases and 11 deaths due to Covid-19. When the lockdown ended 68 days later on 31st May 2020, India reported 190,609 cases and 5,408 deaths.
While millions of livelihoods were lost and a serious migrant and economic crisis emerged, India did manage to “flatten the curve”. Active cases that were increasing at a rate of about 15 per cent in early April came down to about 4 per cent when the lockdown was lifted. This allowed healthcare and ancillary capacity to be built, which saved lives. What also saved lives was the service and shared experience of physicians and healthcare workers. Even in the absence of any specific treatments, open sharing of clinical experience and protocols allowed ICU admissions and mortality rates to decrease with time. Besides increasing capacity, a flatter pandemic curve also saved lives due to accumulated clinical experience and the dedication of healthcare workers. By early February 2021 the Indian Medical Association reported the loss of 734 doctors to Covid-19.
Could India have done better? There have been suggestions that India lost valuable preparatory time in February and March 2020. Some others differ on the timing of the lockdown. Still others think the government relied more on administrative inputs than on scientific advice. These discussions are not just academic. An analysis will help us to be better prepared in future.
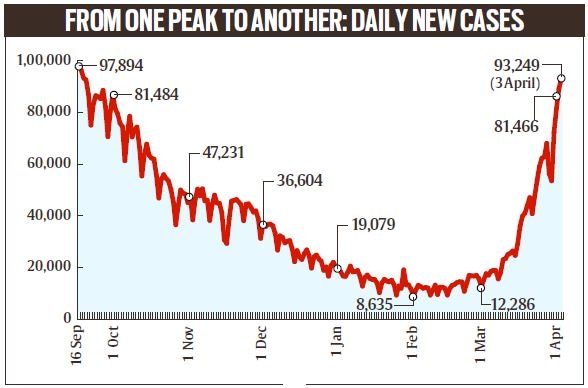
India now has about 12.5 million cases that are globally the third highest, and about 164,000 reported deaths. After reaching a peak in mid-September, there was a steady decline till mid-February 2021, but cases are again on the rise again with 1.01 lakh cases reported on April 4, 2021, which is close to the peak of 97,894 cases on September 16, 2020. The daily rate of infection, which was steady at about 0.1 per cent for a few months has now increased to about 0.6 per cent. But the mortality rate is still low and steady. With over 90 per cent new cases coming from only ten states, what is driving this second wave? Seroprevalence studies have shown protective antibodies in 35 to 40 per cent people in major cities and 10 to 20 per cent in rural areas. The immunity being non-uniform there are pockets of susceptible people in cities as well as villages.
In Maharashtra for example, which is reporting over 60 per cent of India’s cases at this time, about 25 per cent of these cases are coming from the Vidarbha region that was largely spared in the first wave, but 10 per cent cases are also coming from the Pune region that already showed high antibody seroprevalence.
Rapidly falling cases over five months and a relatively low rate of mortality have also led to a low private cost of illness, which contributes to low compliance with masks and distancing. Emerging mutants and variant viruses have also been suggested as driving this surge. Variants of concern, including those that have contributed to increased spread in UK, South Africa and Brazil, as well as home-grown variant viruses are increasingly being found in India. It remains to be seen if these are linked to the present surge.
Curbing a pandemic with vaccines
For the first time in the history of human infectious diseases, a vaccine is being deployed to curb a pandemic. Developments in science and technology over the past two decades made it possible to know the genetic sequence of the new virus within one week of its emergence. To compare, it took over 80 years to decipher the full genetic sequence of the 1918 pandemic flu virus. It took over four months to establish the causative agent for the 2002-03 SARS outbreak.
The availability of genetic sequences of SARS-CoV2 in early January started a race to develop Covid-19 vaccines. Moderna, a ten-year-old company, developed a vaccine based on the novel mRNA platform and started its clinical testing only 63 days after the sequence became available. A similar vaccine invented at a young German company called BioNTech and licensed to Pfizer, was the first to get approval on December 11, 2020, well within 12 months of the discovery of the new disease and nine months since it was declared a pandemic. Vaccines typically require years to develop, but in 2020, scientists produced safe and effective vaccines against Covid-19 in record time. There are currently 78 vaccines undergoing clinical testing on humans, of which 13 have received conditional or full approval.
A pandemic vaccine must do three things. First, it should be used to protect healthcare and other frontline workers. Second, it should decrease mortality. And finally, it must be deployed widely to end the pandemic. Most estimates suggest that about 65 to 70 per cent of the population would require infection or vaccination to reach ‘herd immunity’. Crucial evidence of this comes from Israel, where over 75 per cent of people above 60 years of age have received both doses of a mRNA vaccine. For this age group, new positive cases and hospitalizations in Israel have decreased to near baseline levels. The USA, which has the highest load of Covid-19 cases has also committed itself to a vigorous vaccine rollout. The new President promised 100 million vaccine doses in his first 100 days; 121 million doses have already been administered in two months. Covid rates have flattened or declined in all four countries where enough vaccines have been deployed to cover at least 25 per cent of the population; these include Israel, UAE, Maldives and Seychelles.
However, vaccine access and equity have been a challenge. A small group of countries have access to 60 per cent of the vaccines. The European Union has refused to share vaccines manufactured there with COVAX, a global consortium set up to supply vaccines to low and middle income countries (LMICs). In light of such vaccine nationalism, India’s vaccine diplomacy has been a breath of fresh air. Called “Vaccine Maitri”, it has supplied over 65 million vaccine doses to 72 LMICs. This includes vaccine gifts as well as commercial partnerships.
India’s vaccine challenges and the way forward
India’s vaccination plan, also based on the above three-point principle, is to vaccinate 300 million people in the first tranche. This includes 10 million healthcare workers, 20 million frontline workers and 270 million people above 60 years of age and those younger but with significant comorbidities. From April 1, 2021 everyone 45 years of age or older is also eligible for vaccination. About 76 million doses have been administered till now.
India was already a vaccine manufacturing powerhouse before the arrival of this pandemic. It supplied over 60 per cent of global childhood vaccines, including up to 90 per cent of the world’s measles vaccines. It produced about 3 billion vaccine doses annually, of which about 1 billion was used domestically and the remaining 2 billion exported. Two Covid-19 vaccines have received Emergency Use Authorization (EUA) in India and several others are being tested. To vaccinate 300 million Indians in the first phase would require two things – 600 million vaccine doses and a high rate of vaccine administration. Since January 16, when vaccination started in India, about one million doses on an average have been administered daily, but in the past two weeks the daily rate has increased to around two million doses. Still, only 4.8 per cent and 0.7 per cent of Indians have received one or both vaccine doses, respectively. At this rate, it would take nine months to fully vaccinate 20 per cent of India (~ 275 million people) with two doses. The challenge, therefore, is to increase the rate of vaccine administration. This requires increase in vaccine supply, more administration points and convincing people willing to take the vaccines.
With only two vaccines approved in India – Covishield from Serum Institute of India (SII) and Covaxin from Bharat Biotech India Limited (BBIL), is there enough supply? Though India was to have access to 500 million doses of Covishield and about 300 million doses of the Covaxin, there appear to be supply issues to honour both domestic and international commitments. Data shows that so far Covaxin accounts for less than 10 per cent of administered vaccine doses. This lopsided supply is problematic, especially when media reports suggest that SII is not able to meet the local and export demand for Covishield.
The Indian regulator should consider approving at least two other vaccines that have finished efficacy trials and are approved elsewhere, and have partnerships with Indian vaccine companies. The Johnson & Johnson single-dose vaccine showed an efficacy of up to 72 per cent and has received EUA in Bahrain, EU and USA. The company has a partnership with the Hyderabad-based Biologicals E. Russia’s Sputnik V vaccine reported an efficacy of 91.6 per cent and received EUA in Russia and several Asian, African and Latin American countries. This has a partnership with the Hyderabad-based Dr. Reddy’s Labs. A protein nanoparticle vaccine developed by Novavax (USA) reported an efficacy of 96 per cent in USA but only 49 per cent in South Africa due to the circulation of a variant virus. Though it also has a manufacturing agreement of over 1.5 billion doses with SII, this has not yet been approved in any other country. If Covishield could be approved in India without bridging trials and Covaxin without efficacy data, at least two other vaccines can also receive EUA to boost the supply chain.
On any given day, India has 40,000 to 45,000 vaccine administration points. With about 2 million daily vaccinations, these are delivering on average about 50 doses daily, which is half of the planned 100 doses per site per day. With 74.2 million registrations so far, of which almost 55 per cent are walk-ins, the problem appears to be both capacity and vaccine hesitancy. The capacity can increase with more vaccination points, especially in rural areas, and with increased vaccine supply discussed above. Vaccine hesitancy is fuelled by multiple factors that all point to poor communication, mixed messaging and the inability to effectively counter false information. For example, recent reports of blood clots and a pause in use of the Oxford/AstraZeneca vaccine (the same as Covishield) by a number of European countries has created fear in India, where this vaccine has been used in over 90 per cent vaccinations. Though the European Medicines Agency and World Health Organization have found no links between blood clots and the vaccine, time and effective communication will be required to repair the damage.
Science and the future
The global response to Covid-19 reveals the power of science and partnerships. Within days of its notification, viruses were isolated from patients and characterized, which paved the way for developing diagnostic tests, vaccines and therapies. With almost one million SARS-CoV-2 genomic sequences publicly available by now, it allows scientists to model its evolution and movement across the globe. Multiple vaccines were developed, tested and approved within a year. This is remarkable considering that in 2003 it took 20 months for the SARS vaccine to reach testing. Over 1100 diagnostic tests have been developed and evaluated, 24 different treatments are in use with various levels of efficacy, and more than 110,000 publications on Covid-19 are openly accessible. This remarkable speed and collaboration have created societal value for science and saved lives.
However, the scientific process remains poorly understood. The blood clots scare shows how association is confused with causality. The US Centers for Disease Control and Prevention (CDC) reports that 1 person in 1000 randomly develop blood clots every year. If a blood clot will be associated with a new vaccine within one month of vaccination, let us divide this number by 12. The incidence is 0.08 per 1000 people per month. The European Union reported 30 cases of blood clots after vaccinating 5 million people, which works out to be 0.006, i.e., 13 times less than random chance. Another way to establish causality is to compare the incidence of blood clots in people who blindly and randomly received the vaccine versus those who got a placebo. This was done in phase 3 trials. The incidence of blood clots in both vaccine and placebo groups was rare and not statistically different. This is the scientific method. Everything else is scaremongering.
How will the pandemic play out this year and in the future? That will depend on vaccine availability, coverage and duration of protection. Models of global vaccine manufacturing and capacity show that Covid-19 vaccines sufficient to cover all those vulnerable and at risk would only be available by mid-2022 and for everyone by mid- to late-2023. There is also a problem of unequal access. The poorest countries may only be able to achieve 20 per cent coverage through vaccines provided by the COVAX partnership. The duration of vaccine-mediated protection may be gauged from studies following natural infection. Neutralizing antibodies wane off in about 3 to 5 months but cell-mediated immune response lasts longer. Infection by other endemic human coronaviruses may also offer some protection. Modelling studies by researchers at Harvard University have suggested various scenarios – annual winter outbreaks if immunity lasts less than 40 weeks; outbreaks every other year if immunity is longer than 100 weeks; winter outbreaks if transmission is seasonal; or elimination by 2024 if there is cross-protection from exposure to endemic coronaviruses. While these models have assumed seasonal variation like in influenza viruses, which is driven by genetic drift, SARS-CoV-2 is genetically much more stable. As we have already seen, pandemic waves remain difficult to predict.
Emerging viral variants have added to the complexity. At least three widely circulating variant lineages – called the UK (B.1.1.7), South African (B.1.351) and Brazil (P.1) lineages have emerged with variable consequences. Trials have already shown compromised efficacy of existing vaccines against viruses of the South African and Brazil lineages, prompting vaccine companies to go back to the drawing board. With increasing vaccine coverage globally, there would be fewer opportunities for transmission and this will reduce the virulence or disease-causing potential of SARS-CoV2. Increasing vaccine coverage would also lead to evolutionary pressure on the virus to develop vaccine-escape mutants, which are observed for other viruses following widespread vaccination.
However, since this will involve changing the virus-cell binding interface, it may also lead to less fit and less virulent viruses. These scenarios should be monitored closely over the next few years through characterization of viruses from infected people. Increased genomic sequencing will also allow us to catch variants that spread faster or cause more severe outcomes well in time.
Science has shown the way by fast-tracking Covid-19 vaccines. We must do more by way of better communications and building trust to assure the public that the vaccines are safe and effective. For the first time in the history of human disease, we have the historic opportunity to end a pandemic through vaccines.
Epilogue
Unlike old plagues and pandemics, the fear today is fed more by our understanding of disease than of the unknown. “Fear, like the thought of dying, makes us feel alone, but the recognition that we are all experiencing a similar anguish draws us out of our loneliness,” says Pamuk. He further adds, “We are no longer mortified by our fear; we discover a humility in it that encourages mutual understanding”.
“Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us,” says author Arundhati Roy, adding, “And in the midst of this terrible despair, it offers us a chance to rethink the doomsday machine we have built for ourselves. Nothing could be worse than a return to normality.”
We are at an inflection point in our shared history. Will we learn from it for a better future?
The expert
Dr Shahid Jameel is currently director of Trivedi School of Biosciences at Ashoka University. He has previously worked with the Delhi-based International Centre for Genetic Engineering and Biotechnology (ICGEB), and served as chief executive of the Wellcome Trust/DBT Alliance which funds health research.
Source: Read Full Article